Sunday Poster Session
Category: Biliary/Pancreas
P0077 - Metabolic Mayhem: Pancreatic Insulinoma Masquerading as Altered Mental Status
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- LD
Lauren Davis, DO
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Lauren Davis, DO, Stefanie Gallagher, DO, Julianna Tantum, DO, Keith Lee, DO, Dina Green, MD, Rita El-Hajj, MD, Rebecca Heintzelman, MD, Kristen Lott, MD, Malini Mathur, MD
Lankenau Medical Center, Wynnewood, PA
Introduction: Insulinomas are rare pancreatic neuroendocrine tumors that hypersecrete insulin leading to hypoglycemia. We present a patient with altered mental status, found to have refractory hypoglycemia diagnosed with an insulinoma despite negative imaging. This case highlights the importance of a high clinical suspicion to arrive at this diagnosis promptly to enable treatment and decrease morbidity and mortality.
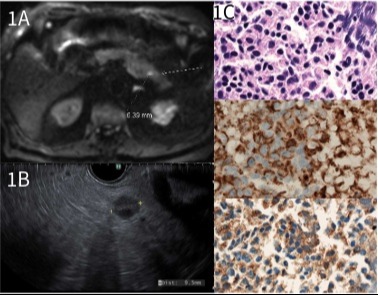
Case Description/Methods: A 79-year-old transgender female with history of frequent urinary tract infections (UTI) presented with altered mental status, initially thought to be secondary to recurrent UTI and antibiotics were initiated. On arrival, she was hypoglycemic with blood glucose (BG) of 49 mg/dL with subsequent course complicated by persistent hypoglycemia despite dextrose-containing fluids. She reported one-year history of episodic hypoglycemic symptoms, resolving with oral intake. Labs showed abnormally elevated C-peptide of 2.58 and insulin of 6.7 with BG of 49, suggestive of inappropriate insulin secretion. ACTH, cortisol, sulfonylurea/meglinitide, IGF-1 and IGF-2 were all unremarkable. CT with normal pancreas. MRI abdomen with mild focus of restricted diffusion in pancreatic tail but no pancreatic mass (Figure 1A). Patient underwent EUS showing 10 mm hypoechoic round pancreatic tail mass (Figure 1B). Fine needle aspiration performed with cytology consistent with well-differentiated neuroendocrine tumor, suggestive of insulinoma (Figure 1C). Patient discharged with close surgical follow-up.
Discussion: Insulinomas are rare neuroendocrine tumors characterized by insulin hypersecretion leading to hypoglycemia. Although they are most commonly benign, their effect can be lethal causing both fasting and postprandial hypoglycemia. Diagnosis begins with biochemical testing by measuring insulin, C-peptide, pro-insulin, and beta hydroxybutyrates levels during a hypoglycemic episode. CT scan is often the next step in diagnosis. However, up to 80% of insulinomas are smaller than 2 cm in size and unable to be localized on CT. MRI can detect up to 85% of insulinomas. In our case, imaging showed no pancreatic mass. If imaging is negative and suspicion remains high, endoscopic ultrasonography can be useful in diagnosis to locate small tumors. Treatment of insulinomas is surgical resection with 90% cure rate. After extensive literary research, this is the only case report of a patient misdiagnosed with a UTI and found to have insulinoma despite initial negative imaging.
Disclosures:
Lauren Davis, DO, Stefanie Gallagher, DO, Julianna Tantum, DO, Keith Lee, DO, Dina Green, MD, Rita El-Hajj, MD, Rebecca Heintzelman, MD, Kristen Lott, MD, Malini Mathur, MD. P0077 - Metabolic Mayhem: Pancreatic Insulinoma Masquerading as Altered Mental Status, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Insulinomas are rare pancreatic neuroendocrine tumors that hypersecrete insulin leading to hypoglycemia. We present a patient with altered mental status, found to have refractory hypoglycemia diagnosed with an insulinoma despite negative imaging. This case highlights the importance of a high clinical suspicion to arrive at this diagnosis promptly to enable treatment and decrease morbidity and mortality.
Case Description/Methods: A 79-year-old transgender female with history of frequent urinary tract infections (UTI) presented with altered mental status, initially thought to be secondary to recurrent UTI and antibiotics were initiated. On arrival, she was hypoglycemic with blood glucose (BG) of 49 mg/dL with subsequent course complicated by persistent hypoglycemia despite dextrose-containing fluids. She reported one-year history of episodic hypoglycemic symptoms, resolving with oral intake. Labs showed abnormally elevated C-peptide of 2.58 and insulin of 6.7 with BG of 49, suggestive of inappropriate insulin secretion. ACTH, cortisol, sulfonylurea/meglinitide, IGF-1 and IGF-2 were all unremarkable. CT with normal pancreas. MRI abdomen with mild focus of restricted diffusion in pancreatic tail but no pancreatic mass (Figure 1A). Patient underwent EUS showing 10 mm hypoechoic round pancreatic tail mass (Figure 1B). Fine needle aspiration performed with cytology consistent with well-differentiated neuroendocrine tumor, suggestive of insulinoma (Figure 1C). Patient discharged with close surgical follow-up.
Discussion: Insulinomas are rare neuroendocrine tumors characterized by insulin hypersecretion leading to hypoglycemia. Although they are most commonly benign, their effect can be lethal causing both fasting and postprandial hypoglycemia. Diagnosis begins with biochemical testing by measuring insulin, C-peptide, pro-insulin, and beta hydroxybutyrates levels during a hypoglycemic episode. CT scan is often the next step in diagnosis. However, up to 80% of insulinomas are smaller than 2 cm in size and unable to be localized on CT. MRI can detect up to 85% of insulinomas. In our case, imaging showed no pancreatic mass. If imaging is negative and suspicion remains high, endoscopic ultrasonography can be useful in diagnosis to locate small tumors. Treatment of insulinomas is surgical resection with 90% cure rate. After extensive literary research, this is the only case report of a patient misdiagnosed with a UTI and found to have insulinoma despite initial negative imaging.
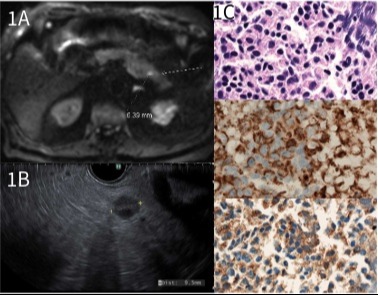
Figure: Figure 1A: MRI Abdomen with contrast, DWI showing a 6 mm focus of restricted diffusion is seen in pancreatic tail. However, no corresponding solid mass is seen on other imaging sequences. Main pancreatic duct is normal in caliber. No evidence of pancreas divisum. Figure 1B: Endoscopic ultrasound image showing a round, hypoechoic, mass identified in the pancreatic tail, measuring 10 mm in maximal cross-sectional diameter. The endosonographic borders were well-defined. Fine needle aspiration for cytology was performed. Figure 1C: Pancreatic Tail FNA: Cells compatible with a well-differentiated neuroendocrine tumor. The specimen is composed of intermediate in size cells with rounded nuclei containing even chromatin and occasional apparent nucleoli with surrounding granular cytoplasm. Some autolysis is noted without overt necrosis. Mitotic figures are not seen (top figure). Immunohistochemical stains performed. The tumor cells show cytoplasmic granular positivity for keratin AE1/AE3 (middle figure) as well as positivity for chromogranin (bottom figure), synaptophysin (weak), INSM1 (patchy) and CK7 (weak, patchy). A proliferation index by Ki-67 is 6.7% (500 cells counted), favoring a grade 2 tumor.
Disclosures:
Lauren Davis indicated no relevant financial relationships.
Stefanie Gallagher indicated no relevant financial relationships.
Julianna Tantum indicated no relevant financial relationships.
Keith Lee indicated no relevant financial relationships.
Dina Green indicated no relevant financial relationships.
Rita El-Hajj indicated no relevant financial relationships.
Rebecca Heintzelman indicated no relevant financial relationships.
Kristen Lott indicated no relevant financial relationships.
Malini Mathur indicated no relevant financial relationships.
Lauren Davis, DO, Stefanie Gallagher, DO, Julianna Tantum, DO, Keith Lee, DO, Dina Green, MD, Rita El-Hajj, MD, Rebecca Heintzelman, MD, Kristen Lott, MD, Malini Mathur, MD. P0077 - Metabolic Mayhem: Pancreatic Insulinoma Masquerading as Altered Mental Status, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
