Sunday Poster Session
Category: Biliary/Pancreas
P0083 - Mass Effect Due to Extensive Choledocholithiasis and Biliary Ductal Dilation: An Unusual Cause of Portal Vein Thrombosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmed Abidali, DO
Abrazo Health
Glendale, AZ
Presenting Author(s)
Ahmed Abidali, DO1, Samier Deen, DO2, Vanessa F. Eller, MD3, Mustafa Nawaz, DO3, Kevin Liu, MD3, Rohit Nathan, DO3
1Abrazo Health, Glendale, AZ; 2HonorHealth, Scottsdale, AZ; 3University of Arizona College of Medicine, Phoenix, AZ
Introduction: Portal vein thrombosis (PVT) is an infrequent occurrence in the absence of liver cirrhosis, malignancy, or a hypercoagulable state. Although rare, PVT can arise in the setting of extensive choledocholithiasis and biliary ductal dilation due to associated inflammation and venous outflow impedance. In such cases, treatment should emphasize common bile duct (CBD) stone removal and stent placement via ERCP in an effort to reduce stone burden and hasten PVT resolution.
Case Description/Methods: A 60-year-old female with a medical history significant for cholecystectomy (2015) presented with acute on chronic abdominal pain, subjective fevers, and chills. On arrival, she was admitted to the ICU for septic shock secondary to cholangitis and initiated on vasopressors and broad-spectrum antibiotics. Initial labs were significant for WBC 31.8 K/uL, AST 132 U/L, ALT 55 U/L, ALP 231 IU/L, and total bilirubin 2.8 mg/dL. CT abdomen and pelvis with IV contrast revealed extensive and diffuse intra- and extrahepatic biliary ductal dilation, hepatosplenomegaly, central and left PVT with complete thrombosis of the left portal vein. She underwent ERCP with biliary sphincterotomy, balloon sweep sludge extraction and CBD stent placement. Due to tenuous hemodynamics, the CBD was not aggressively swept for stone extraction. A repeat ERCP with EUS revealed distal CBD stricture and retained stones. Electrohydraulic lithotripsy was performed for stone fragmentation followed by stone removal via balloon extraction and stent replacement. Distal CBD brushing sample was negative for malignancy. A follow up CT demonstrated resolution of PVT, and interval improvement in intra- and extrahepatic ductal dilation, and hepatosplenomegaly. A repeat outpatient ERCP for intended residual stone clearance revealed extensive choledocholithiasis with over 30 stones removed via SpyBasket retrieval and balloon sweep. The previously placed plastic stent was replaced by a metal stent. A final repeat ERCP confirmed absence of stones, resolution of CBD stricture, and metal stent which was then removed.
Discussion: The pathogenesis of PVT in this patient is thought to be due to mass effect from venous compression and inflammatory ductal changes in the setting of profound stone burden. Although anticoagulation is often recognized as the mainstay treatment of PVT, this case demonstrates bile duct stone removal to be a safe and viable therapeutic strategy in patients with PVT due to bile duct obstruction.

Disclosures:
Ahmed Abidali, DO1, Samier Deen, DO2, Vanessa F. Eller, MD3, Mustafa Nawaz, DO3, Kevin Liu, MD3, Rohit Nathan, DO3. P0083 - Mass Effect Due to Extensive Choledocholithiasis and Biliary Ductal Dilation: An Unusual Cause of Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Abrazo Health, Glendale, AZ; 2HonorHealth, Scottsdale, AZ; 3University of Arizona College of Medicine, Phoenix, AZ
Introduction: Portal vein thrombosis (PVT) is an infrequent occurrence in the absence of liver cirrhosis, malignancy, or a hypercoagulable state. Although rare, PVT can arise in the setting of extensive choledocholithiasis and biliary ductal dilation due to associated inflammation and venous outflow impedance. In such cases, treatment should emphasize common bile duct (CBD) stone removal and stent placement via ERCP in an effort to reduce stone burden and hasten PVT resolution.
Case Description/Methods: A 60-year-old female with a medical history significant for cholecystectomy (2015) presented with acute on chronic abdominal pain, subjective fevers, and chills. On arrival, she was admitted to the ICU for septic shock secondary to cholangitis and initiated on vasopressors and broad-spectrum antibiotics. Initial labs were significant for WBC 31.8 K/uL, AST 132 U/L, ALT 55 U/L, ALP 231 IU/L, and total bilirubin 2.8 mg/dL. CT abdomen and pelvis with IV contrast revealed extensive and diffuse intra- and extrahepatic biliary ductal dilation, hepatosplenomegaly, central and left PVT with complete thrombosis of the left portal vein. She underwent ERCP with biliary sphincterotomy, balloon sweep sludge extraction and CBD stent placement. Due to tenuous hemodynamics, the CBD was not aggressively swept for stone extraction. A repeat ERCP with EUS revealed distal CBD stricture and retained stones. Electrohydraulic lithotripsy was performed for stone fragmentation followed by stone removal via balloon extraction and stent replacement. Distal CBD brushing sample was negative for malignancy. A follow up CT demonstrated resolution of PVT, and interval improvement in intra- and extrahepatic ductal dilation, and hepatosplenomegaly. A repeat outpatient ERCP for intended residual stone clearance revealed extensive choledocholithiasis with over 30 stones removed via SpyBasket retrieval and balloon sweep. The previously placed plastic stent was replaced by a metal stent. A final repeat ERCP confirmed absence of stones, resolution of CBD stricture, and metal stent which was then removed.
Discussion: The pathogenesis of PVT in this patient is thought to be due to mass effect from venous compression and inflammatory ductal changes in the setting of profound stone burden. Although anticoagulation is often recognized as the mainstay treatment of PVT, this case demonstrates bile duct stone removal to be a safe and viable therapeutic strategy in patients with PVT due to bile duct obstruction.

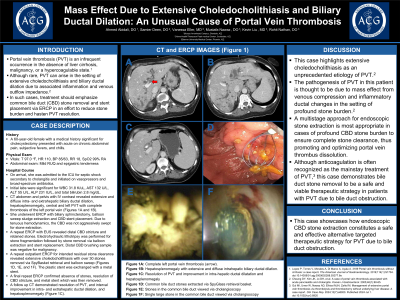
Figure: Panel A: Complete left portal vein thrombosis (arrow).
Panel B: Hepatosplenomegaly with extensive and diffuse intrahepatic biliary ductal dilation.
Panel C: Common bile duct stones extracted via SpyGlass retrieval basket.
Panel B: Hepatosplenomegaly with extensive and diffuse intrahepatic biliary ductal dilation.
Panel C: Common bile duct stones extracted via SpyGlass retrieval basket.
Disclosures:
Ahmed Abidali indicated no relevant financial relationships.
Samier Deen indicated no relevant financial relationships.
Vanessa Eller indicated no relevant financial relationships.
Mustafa Nawaz indicated no relevant financial relationships.
Kevin Liu indicated no relevant financial relationships.
Rohit Nathan indicated no relevant financial relationships.
Ahmed Abidali, DO1, Samier Deen, DO2, Vanessa F. Eller, MD3, Mustafa Nawaz, DO3, Kevin Liu, MD3, Rohit Nathan, DO3. P0083 - Mass Effect Due to Extensive Choledocholithiasis and Biliary Ductal Dilation: An Unusual Cause of Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
