Sunday Poster Session
Category: Biliary/Pancreas
P0087 - Autoimmune Pancreatitis as an Atypical Etiology for a Benign Biliary Stricture
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Neev Mehta, MD
Lahey Hospital and Medical Center
Burlington, MA
Presenting Author(s)
Neev Mehta, MD1, Neethi Dasu, DO2, Khaldoon Khirfan, MD3, Mena Bakhit, MD1, Haider Rahman, MD1
1Lahey Hospital and Medical Center, Burlington, MA; 2Beth Israel Lahey Health, Burlington, MA; 3Lahey Clinic, Burlington, MA
Introduction:
Benign bile duct strictures (BBSs) are a rare complication that arises due to postoperative bile duct injury, pancreaticobiliary inflammatory processes, or biliary anastomosis following liver transplantation. The treatment aims to maintain patency of the biliary structure to preserve biliary drainage, prevent cholangitis, and preserve hepatic function. We report an uncommon case of a biliary stricture initially suspected to be cholecystectomy-related, but further evaluation uncovered autoimmune pancreatitis as the underlying etiology.
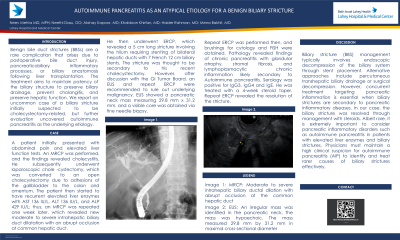
Case Description/Methods: A 74-year-old male patient initially presented with abdominal pain and elevated liver function tests. An MRCP was performed, and the findings revealed cholecystitis. He subsequently underwent laparoscopic cholecystectomy, which was converted to an open cholecystectomy due to adhesions of the gallbladder. The patient then started to have recurrent elevated liver enzymes with AST 136 IU/L, ALT 136 IU/L, and ALP 429 IU/L; thus, an MRCP was repeated, which revealed new moderate to severe intrahepatic biliary duct dilatation with an abrupt occlusion at common hepatic duct. He then underwent ERCP, which revealed a 5 cm long stricture involving the hilum requiring stenting of bilateral hepatic ducts. The stricture was thought to be secondary to his recent cholecystectomy. However, after discussion with the GI Tumor Board, an EUS and repeat ERCP were recommended to rule out underlying malignancy. EUS showed a pancreatic neck mass measuring 29.8 mm x 31.2 mm, and a visible core was obtained via fine needle biopsy. Repeat ERCP was performed then, and brushings for cytology and FISH were obtained. Pathology revealed chronic pancreatitis with glandular atrophy, stromal fibrosis, and lymphoplasmacytic chronic inflammation likely secondary to Autoimmune pancreatitis. Serology was positive for IgG4 and IgE. He was treated with a 4-week steroid taper. Repeat ERCP revealed the resolution of the stricture.
Discussion:
Biliary stricture management typically involves endoscopic decompression of the biliary system. In our case, the biliary stricture was resolved through management with steroids. Albeit rare, it is extremely important to consider pancreatic inflammatory disorders such as autoimmune pancreatitis in patients with elevated liver enzymes and biliary strictures. Physicians must maintain a high clinical suspicion for autoimmune pancreatitis (AIP) to identify and treat rarer causes of biliary strictures effectively.
Disclosures:
Neev Mehta, MD1, Neethi Dasu, DO2, Khaldoon Khirfan, MD3, Mena Bakhit, MD1, Haider Rahman, MD1. P0087 - Autoimmune Pancreatitis as an Atypical Etiology for a Benign Biliary Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lahey Hospital and Medical Center, Burlington, MA; 2Beth Israel Lahey Health, Burlington, MA; 3Lahey Clinic, Burlington, MA
Introduction:
Benign bile duct strictures (BBSs) are a rare complication that arises due to postoperative bile duct injury, pancreaticobiliary inflammatory processes, or biliary anastomosis following liver transplantation. The treatment aims to maintain patency of the biliary structure to preserve biliary drainage, prevent cholangitis, and preserve hepatic function. We report an uncommon case of a biliary stricture initially suspected to be cholecystectomy-related, but further evaluation uncovered autoimmune pancreatitis as the underlying etiology.
Case Description/Methods: A 74-year-old male patient initially presented with abdominal pain and elevated liver function tests. An MRCP was performed, and the findings revealed cholecystitis. He subsequently underwent laparoscopic cholecystectomy, which was converted to an open cholecystectomy due to adhesions of the gallbladder. The patient then started to have recurrent elevated liver enzymes with AST 136 IU/L, ALT 136 IU/L, and ALP 429 IU/L; thus, an MRCP was repeated, which revealed new moderate to severe intrahepatic biliary duct dilatation with an abrupt occlusion at common hepatic duct. He then underwent ERCP, which revealed a 5 cm long stricture involving the hilum requiring stenting of bilateral hepatic ducts. The stricture was thought to be secondary to his recent cholecystectomy. However, after discussion with the GI Tumor Board, an EUS and repeat ERCP were recommended to rule out underlying malignancy. EUS showed a pancreatic neck mass measuring 29.8 mm x 31.2 mm, and a visible core was obtained via fine needle biopsy. Repeat ERCP was performed then, and brushings for cytology and FISH were obtained. Pathology revealed chronic pancreatitis with glandular atrophy, stromal fibrosis, and lymphoplasmacytic chronic inflammation likely secondary to Autoimmune pancreatitis. Serology was positive for IgG4 and IgE. He was treated with a 4-week steroid taper. Repeat ERCP revealed the resolution of the stricture.
Discussion:
Biliary stricture management typically involves endoscopic decompression of the biliary system. In our case, the biliary stricture was resolved through management with steroids. Albeit rare, it is extremely important to consider pancreatic inflammatory disorders such as autoimmune pancreatitis in patients with elevated liver enzymes and biliary strictures. Physicians must maintain a high clinical suspicion for autoimmune pancreatitis (AIP) to identify and treat rarer causes of biliary strictures effectively.
Disclosures:
Neev Mehta indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Khaldoon Khirfan indicated no relevant financial relationships.
Mena Bakhit indicated no relevant financial relationships.
Haider Rahman indicated no relevant financial relationships.
Neev Mehta, MD1, Neethi Dasu, DO2, Khaldoon Khirfan, MD3, Mena Bakhit, MD1, Haider Rahman, MD1. P0087 - Autoimmune Pancreatitis as an Atypical Etiology for a Benign Biliary Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
