Sunday Poster Session
Category: Biliary/Pancreas
P0010 - A Longitudinal Analysis of Cholangiocarcinoma-Related Mortality in the United States
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- NO
Nazli Begum Ozturk, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Nazli Begum Ozturk, MD1, Hoang Nhat Pham, MD2, Leandro Sierra, MD3, Sabrina Ho, MD2, Aarzoo Kumar, BS2, Rama Mouhaffel, MD2, Ramzi Ibrahim, MD2, Ahmet Gurakar, MD, FACG4
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Banner - University of Arizona, Tucson, AZ; 3Cleveland Clinic Foundation, Cleveland, OH; 4Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Cholangiocarcinoma (CCA) is the second most common primary liver malignancy with high rates of mortality. Many studies report increasing rates of both intrahepatic CCA (iCCA) and extrahepatic CCA (eCCA) in the United States (US). We aimed to investigate CCA-related mortality rates between 1999-2020, and to identify the most vulnerable patient populations for death in the US.
Methods: Mortality data was retrieved from multiple cause-of-death files in the CDC repository, using ICD-10 codes for iCCA (C22.1) and eCCA (C24.0, C24.8, C24.9). Age-adjusted mortality rate (AAMR) and 95% confidence interval were compared across demographic and geographic factors. Log-linear regression models were used to analyzed temporal mortality trends, presented as average annual mortality rate (AAPC).
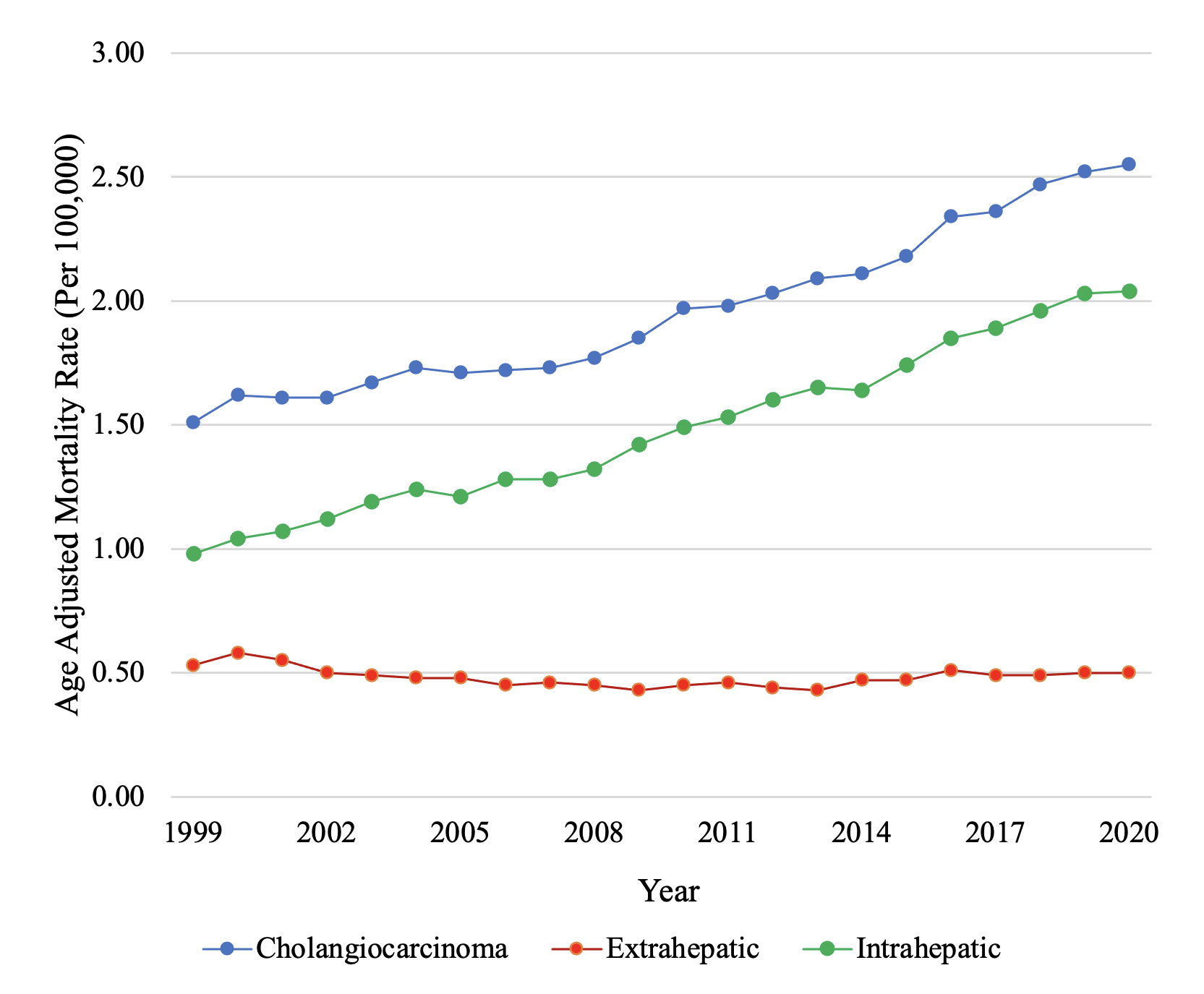
Results: Between 1999-2020, a total of 148,871 CCA-related deaths were identified, with 36,048 deaths due to eCCA and 113,450 deaths due to iCCA. AAMR for was increased from 1.51 [95% CI, 1.46-1.55] in 1999 to 2.55 [2.50-2.60] in 2020 with an AAPC of +2.40%, p< 0.001 (Figure 1). From 1999 to 2020, the annual iCAA mortality rate increased, with AAPC +3.55%, p< 0.001 while annual eCCA mortality remained stable, with AAPC -0.43%, p=0.11. Higher mortality rates were observed in males compared to females for both iCAA (AAMR 1.77 [1.75-1.78] vs 1.35 [1.34-1.36]) and eCAA (AAMR 0.55 [0.54-0.56] vs 0.44 [0.44-0.45]). Higher iCAA mortality rate was observed in Hispanic populations (AAMR 1.75 [1.72 -1.79]) compared to non-Hispanic (AAMR 1.51 [1.50-1.52]) populations, and in urban (AAMR 1.56 [1.55-1.57]) compared to rural (AAMR 1.38 (1.36-1.41]) communities, and was highest among Asian (AAMR 2.05 [2.00-2.10]) populations. There were no observed differences in eCCA mortality rates across racial, ethnic, or urbanization categories. Similar AAMR was observed among 4 US census regions for both iCCA and eCCA.
Discussion: AAMR has increased for both iCCA and eCCA between 1999-2020 in the US. Significant variations were seen across gender, ethnicity, race, and rural-urban settings for iCCA mortality, while no significant differences were seen for eCCA mortality. Further investigations for understanding the epidemiology and risk factors for most vulnerable populations are essential to mitigate health disparities and potentially CCA mortality.
Disclosures:
Nazli Begum Ozturk, MD1, Hoang Nhat Pham, MD2, Leandro Sierra, MD3, Sabrina Ho, MD2, Aarzoo Kumar, BS2, Rama Mouhaffel, MD2, Ramzi Ibrahim, MD2, Ahmet Gurakar, MD, FACG4. P0010 - A Longitudinal Analysis of Cholangiocarcinoma-Related Mortality in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Banner - University of Arizona, Tucson, AZ; 3Cleveland Clinic Foundation, Cleveland, OH; 4Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Cholangiocarcinoma (CCA) is the second most common primary liver malignancy with high rates of mortality. Many studies report increasing rates of both intrahepatic CCA (iCCA) and extrahepatic CCA (eCCA) in the United States (US). We aimed to investigate CCA-related mortality rates between 1999-2020, and to identify the most vulnerable patient populations for death in the US.
Methods: Mortality data was retrieved from multiple cause-of-death files in the CDC repository, using ICD-10 codes for iCCA (C22.1) and eCCA (C24.0, C24.8, C24.9). Age-adjusted mortality rate (AAMR) and 95% confidence interval were compared across demographic and geographic factors. Log-linear regression models were used to analyzed temporal mortality trends, presented as average annual mortality rate (AAPC).
Results: Between 1999-2020, a total of 148,871 CCA-related deaths were identified, with 36,048 deaths due to eCCA and 113,450 deaths due to iCCA. AAMR for was increased from 1.51 [95% CI, 1.46-1.55] in 1999 to 2.55 [2.50-2.60] in 2020 with an AAPC of +2.40%, p< 0.001 (Figure 1). From 1999 to 2020, the annual iCAA mortality rate increased, with AAPC +3.55%, p< 0.001 while annual eCCA mortality remained stable, with AAPC -0.43%, p=0.11. Higher mortality rates were observed in males compared to females for both iCAA (AAMR 1.77 [1.75-1.78] vs 1.35 [1.34-1.36]) and eCAA (AAMR 0.55 [0.54-0.56] vs 0.44 [0.44-0.45]). Higher iCAA mortality rate was observed in Hispanic populations (AAMR 1.75 [1.72 -1.79]) compared to non-Hispanic (AAMR 1.51 [1.50-1.52]) populations, and in urban (AAMR 1.56 [1.55-1.57]) compared to rural (AAMR 1.38 (1.36-1.41]) communities, and was highest among Asian (AAMR 2.05 [2.00-2.10]) populations. There were no observed differences in eCCA mortality rates across racial, ethnic, or urbanization categories. Similar AAMR was observed among 4 US census regions for both iCCA and eCCA.
Discussion: AAMR has increased for both iCCA and eCCA between 1999-2020 in the US. Significant variations were seen across gender, ethnicity, race, and rural-urban settings for iCCA mortality, while no significant differences were seen for eCCA mortality. Further investigations for understanding the epidemiology and risk factors for most vulnerable populations are essential to mitigate health disparities and potentially CCA mortality.
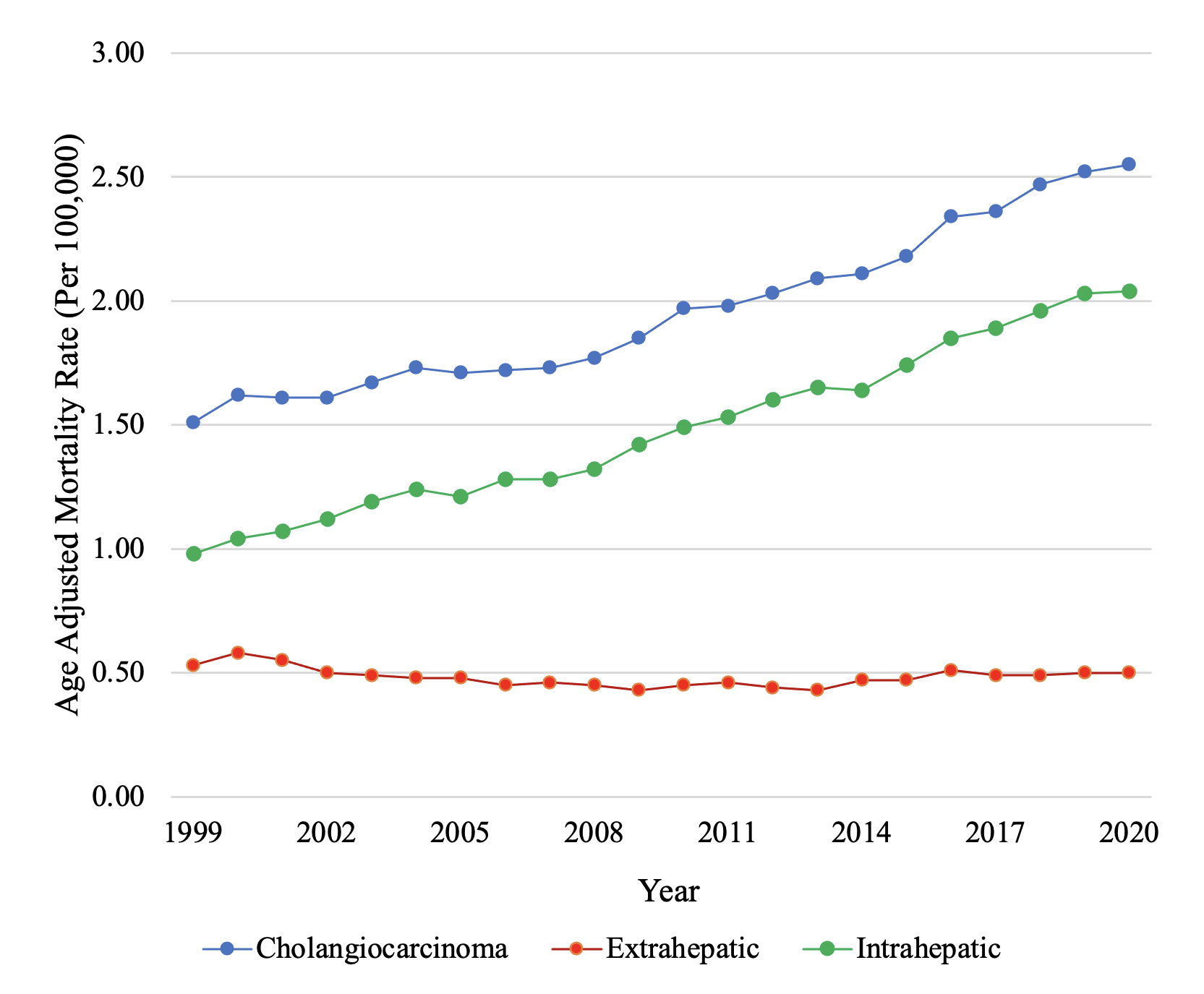
Figure: Figure 1. AAMR for CCA between 1999-2020 in the United States.
Disclosures:
Nazli Begum Ozturk indicated no relevant financial relationships.
Hoang Nhat Pham indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Sabrina Ho indicated no relevant financial relationships.
Aarzoo Kumar indicated no relevant financial relationships.
Rama Mouhaffel indicated no relevant financial relationships.
Ramzi Ibrahim indicated no relevant financial relationships.
Ahmet Gurakar indicated no relevant financial relationships.
Nazli Begum Ozturk, MD1, Hoang Nhat Pham, MD2, Leandro Sierra, MD3, Sabrina Ho, MD2, Aarzoo Kumar, BS2, Rama Mouhaffel, MD2, Ramzi Ibrahim, MD2, Ahmet Gurakar, MD, FACG4. P0010 - A Longitudinal Analysis of Cholangiocarcinoma-Related Mortality in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
