Sunday Poster Session
Category: Biliary/Pancreas
P0018 - Biliary Stenting With and Without Endoscopic Sphincterotomy in Patients With Malignant Biliary Obstruction: Meta-Analysis of Randomized Controlled Trials
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FK
Faisal Kamal, MD
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Aamir Saeed, MD1, Saira Yousuf, MD1, Muhammad Khan, MD2, Manesh Kumar Gangwani, MD3, Muhammad Aziz, MD4, Arnab Ray, MD5, Janak Shah, MD6, Anand Kumar, MD, MPH7, Alexander Schlachterman, MD8, Thomas Kowalski, MD8, Faisal Kamal, MD8
1Vanderbilt University Medical Center, Nashville, TN; 2MD Anderson Cancer Center, Houston, TX; 3University of Toledo, Toledo, OH; 4Bon Secours Mercy, Toledo, OH; 5Ochsner Medical Center, New Orleans, LA; 6Ochsner Health Clinic Foundation, New Orleans, LA; 7Thomas Jefferson University Hospital, Philadelphia, PA; 8Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Endoscopic biliary sphincterotomy (EBS) is commonly performed during ERCP in patients with malignant biliary obstruction (MBO) before stent placement. Studies comparing adverse events between patients with MBO undergoing ERCP with and without EBS have reported conflicting results. We conducted an updated meta-analysis including randomized controlled trials (RCTs) only to evaluate the safety of EBS in these patients and its efficacy in decreasing the risk of PEP
Methods: We reviewed several databases from inception to January 10, 2024, to identify RCTs that compared adverse events of biliary stenting with and without EBS in patients with MBO. Our search strategy included databases including PubMed, Web of Science Core Collection, Embase, and the Cochrane Database of Systematic Reviews. Our outcomes of interest were post-ERCP pancreatitis (PEP), successful stent insertion, and adverse events such as cholangitis, bleeding, perforation, stent migration, and stent occlusion. We calculated pooled risk ratio (RR) with 95% confidence intervals (CI) for all of the outcomes and used a random effect model to analyze the data. Heterogeneity was assessed using the I² statistic
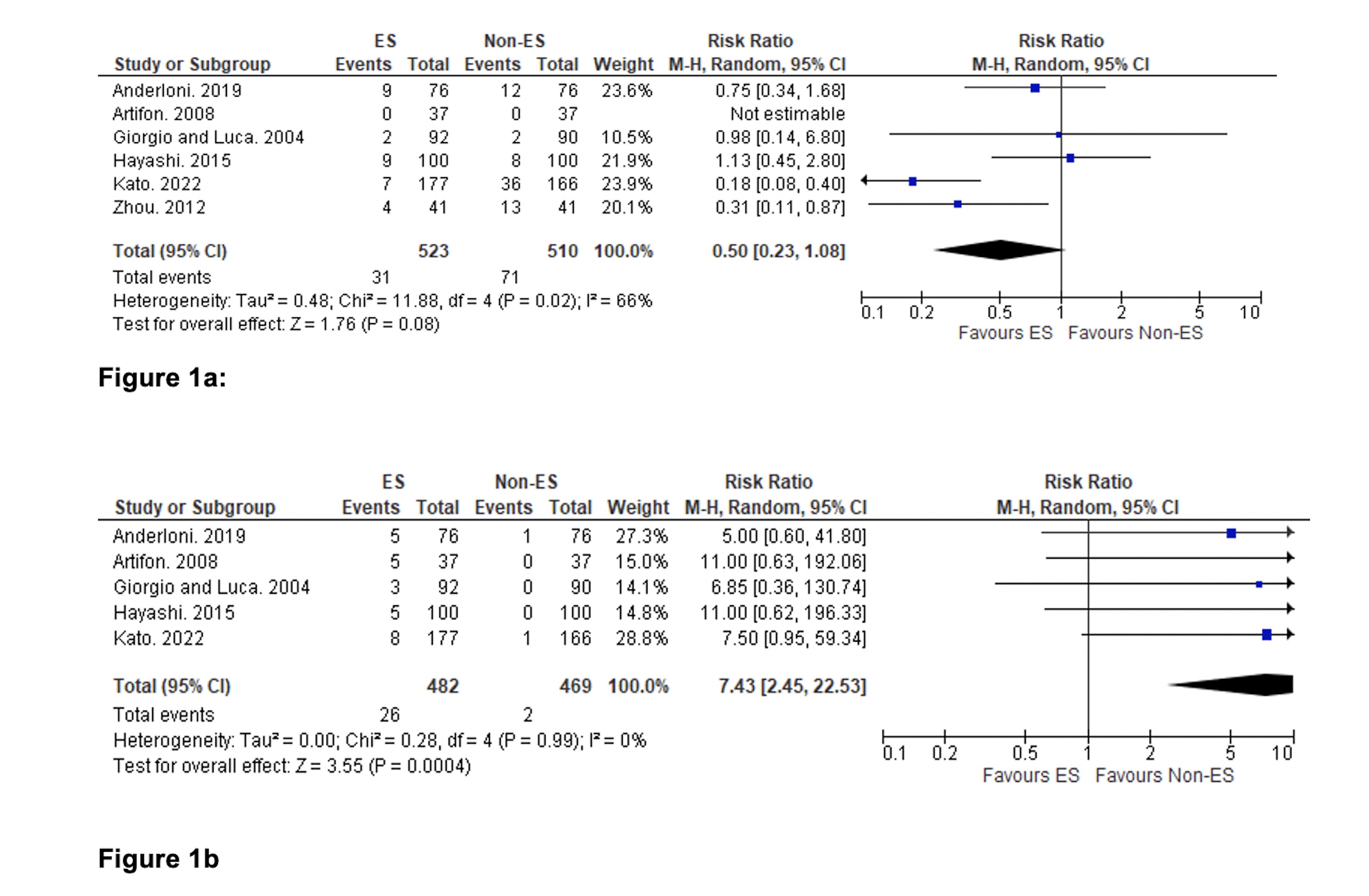
Results: We included 6 RCTs with 1070 patients. There was no significant difference in the rate of PEP between groups, RR (95% CI): 0.50 (0.23-1.08) (Figure 1a). We found no significant difference in the rate of successful stent insertion between groups, RR (95%CI): 1.01 (0.99-1.02). The rate of post-ERCP bleeding was significantly higher in the EBS group, RR (95% CI) 7.43 (2.45-22.53) (Figure 1b). We found no significant difference in rates of other outcomes between groups, such as cholangitis; RR (95%CI): 1.45 (0.64-3.26), I2= 67%, perforation; RR (95% CI): 1.88 (0.07- 47.60) I2= 56%, stent migration; RR (95% CI): 2.30 (0.65, 8.08) I2= 12%, and stent occlusion; RR (95% CI): 0.89 (0.60-1.30), I2= 0% between groups.
Discussion: EBS does not decrease the risk of PEP in patients with MBO and is associated with an increased risk of bleeding.
Disclosures:
Aamir Saeed, MD1, Saira Yousuf, MD1, Muhammad Khan, MD2, Manesh Kumar Gangwani, MD3, Muhammad Aziz, MD4, Arnab Ray, MD5, Janak Shah, MD6, Anand Kumar, MD, MPH7, Alexander Schlachterman, MD8, Thomas Kowalski, MD8, Faisal Kamal, MD8. P0018 - Biliary Stenting With and Without Endoscopic Sphincterotomy in Patients With Malignant Biliary Obstruction: Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Vanderbilt University Medical Center, Nashville, TN; 2MD Anderson Cancer Center, Houston, TX; 3University of Toledo, Toledo, OH; 4Bon Secours Mercy, Toledo, OH; 5Ochsner Medical Center, New Orleans, LA; 6Ochsner Health Clinic Foundation, New Orleans, LA; 7Thomas Jefferson University Hospital, Philadelphia, PA; 8Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Endoscopic biliary sphincterotomy (EBS) is commonly performed during ERCP in patients with malignant biliary obstruction (MBO) before stent placement. Studies comparing adverse events between patients with MBO undergoing ERCP with and without EBS have reported conflicting results. We conducted an updated meta-analysis including randomized controlled trials (RCTs) only to evaluate the safety of EBS in these patients and its efficacy in decreasing the risk of PEP
Methods: We reviewed several databases from inception to January 10, 2024, to identify RCTs that compared adverse events of biliary stenting with and without EBS in patients with MBO. Our search strategy included databases including PubMed, Web of Science Core Collection, Embase, and the Cochrane Database of Systematic Reviews. Our outcomes of interest were post-ERCP pancreatitis (PEP), successful stent insertion, and adverse events such as cholangitis, bleeding, perforation, stent migration, and stent occlusion. We calculated pooled risk ratio (RR) with 95% confidence intervals (CI) for all of the outcomes and used a random effect model to analyze the data. Heterogeneity was assessed using the I² statistic
Results: We included 6 RCTs with 1070 patients. There was no significant difference in the rate of PEP between groups, RR (95% CI): 0.50 (0.23-1.08) (Figure 1a). We found no significant difference in the rate of successful stent insertion between groups, RR (95%CI): 1.01 (0.99-1.02). The rate of post-ERCP bleeding was significantly higher in the EBS group, RR (95% CI) 7.43 (2.45-22.53) (Figure 1b). We found no significant difference in rates of other outcomes between groups, such as cholangitis; RR (95%CI): 1.45 (0.64-3.26), I2= 67%, perforation; RR (95% CI): 1.88 (0.07- 47.60) I2= 56%, stent migration; RR (95% CI): 2.30 (0.65, 8.08) I2= 12%, and stent occlusion; RR (95% CI): 0.89 (0.60-1.30), I2= 0% between groups.
Discussion: EBS does not decrease the risk of PEP in patients with MBO and is associated with an increased risk of bleeding.
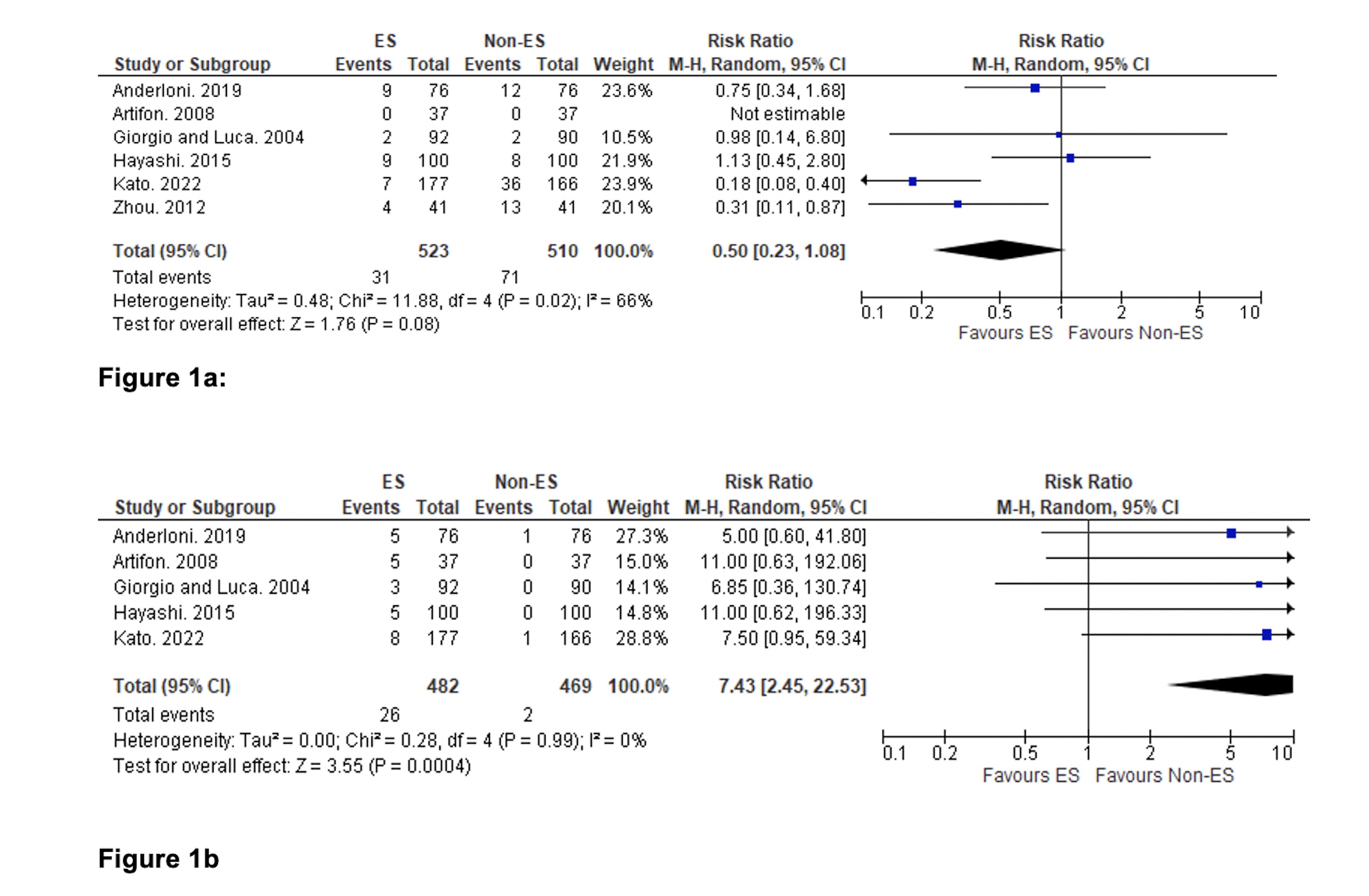
Figure: Comparison of PEP (figure 1a) and post-sphincterotomy bleeding (figure 1b) between groups
Disclosures:
Aamir Saeed indicated no relevant financial relationships.
Saira Yousuf indicated no relevant financial relationships.
Muhammad Khan indicated no relevant financial relationships.
Manesh Kumar Gangwani indicated no relevant financial relationships.
Muhammad Aziz indicated no relevant financial relationships.
Arnab Ray indicated no relevant financial relationships.
Janak Shah indicated no relevant financial relationships.
Anand Kumar: Boston Scientific – Consultant. Olympus – Consultant.
Alexander Schlachterman: Boston Scientific – Consultant. Fuji – Consultant. Laborie – Consultant. Lumendi – Consultant. Olympus – Consultant.
Thomas Kowalski: Boston Scientific – Consultant.
Faisal Kamal indicated no relevant financial relationships.
Aamir Saeed, MD1, Saira Yousuf, MD1, Muhammad Khan, MD2, Manesh Kumar Gangwani, MD3, Muhammad Aziz, MD4, Arnab Ray, MD5, Janak Shah, MD6, Anand Kumar, MD, MPH7, Alexander Schlachterman, MD8, Thomas Kowalski, MD8, Faisal Kamal, MD8. P0018 - Biliary Stenting With and Without Endoscopic Sphincterotomy in Patients With Malignant Biliary Obstruction: Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
