Sunday Poster Session
Category: Biliary/Pancreas
P0019 - Laser-Cut-Type vs Braided-Type Self-Expandable Metallic Stents for Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FK
Faisal Kamal, MD
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Aamir Saeed, MD1, Saira Yousuf, MD1, Muhammad Hayat, MD1, Marjan Haider, MD2, Manesh Kumar Gangwani, MD3, Muhammad Aziz, MD4, Umar Hayat, MD5, Umer Farooq, MD6, Nasir Saleem, MD7, Faisal Kamal, MD8
1Vanderbilt University Medical Center, Nashville, TN; 2Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 3University of Toledo, Toledo, OH; 4Bon Secours Mercy, Toledo, OH; 5Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 6SSM Health Saint Louis University Hospital, St. Louis, MO; 7Indiana University School of Medicine, Indianapolis, IN; 8Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Self-expandable metallic stents (SEMS) are widely used for malignant biliary obstruction (MBO). Laser cut and braided stents are two commonly used types of SEMS, and it is unclear if one stent type is superior to the other. We conducted a systematic review and meta-analysis to compare outcomes of these two stent types in patients with MBO.
Methods: Several databases were reviewed from inception to May 24th, 2024 to identify studies comparing outcomes of laser-cut and braided-type SEMS in patients with MBO. The databases searched included PubMed, Web of Science Core Collection, Embase, and the Cochrane Database of Systematic Reviews. Our outcomes of interest included technical success, clinical success, mean procedure time and adverse events such as pancreatitis, cholecystitis, stent migration and recurrent biliary obstruction. We calculated risk ratios (RRs) with 95% confidence intervals (CIs) for all dichotomous variables and mean difference with 95% CI for continuous variables. Data was analyzed using random effect model. Heterogeneity was assessed using I2 statistic.
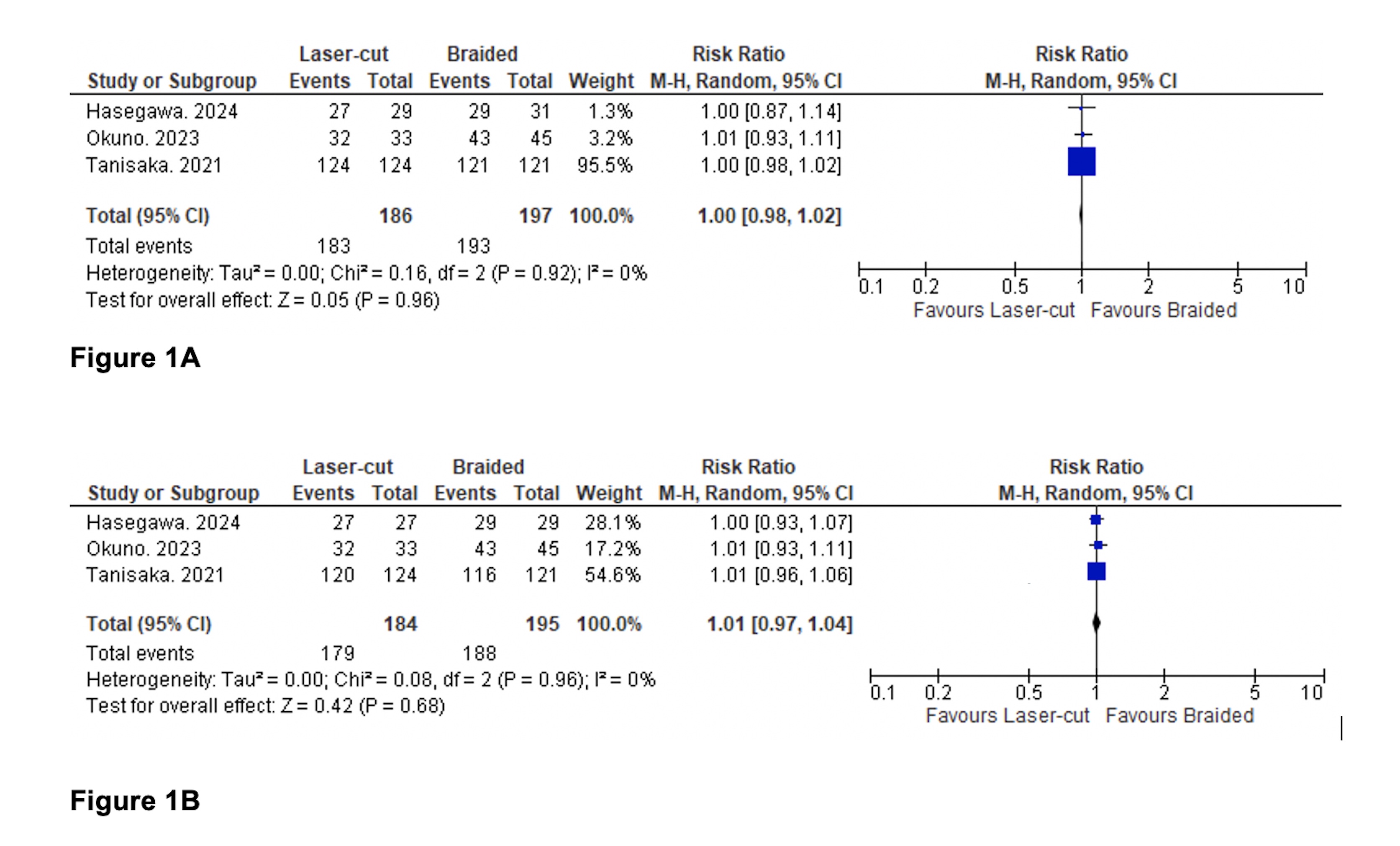
Results: Four studies comprising 430 patients (Laser-cut 210 and braided type 220) met the inclusion criteria. We found no significant difference in rate of technical success, RR (95% CI): 1.00 (0.98,1.02), p=0.96, and clinical success, RR (95% CI): 1.01 (0.97, 1.04), p=0.68 between groups (Figure 1A and B). There was no significant difference in rate of adverse events between groups, RR (95% CI): 1.06 (0.60,1.90), p=0.84 (Figure 3). There was no significant difference in rate of adverse events between groups, such as pancreatitis, RR (95% CI): 01.26(0.59, 2.71), p=0.55; cholecystitis, RR (95% CI): 0.76 (0.30, 1.95), p=0.57; stent migration, RR (95% CI): 1.43(0.32,6.38), p=0.64 and recurrent biliary obstruction RR (95% CI): 1.18 (0.64, 2.16), p=0.60 (Figure 4,5). We found no significant difference in procedure time between groups, MD (95% CI): 0.84(-4.29,5.99), p=0.75 (Figure 6,7).
Discussion: We found no significant difference in outcomes between laser cut and braided stents in patients with MBO. Large multicenter, randomized controlled trials comparing the two stent types are required to further validate these findings.
Disclosures:
Aamir Saeed, MD1, Saira Yousuf, MD1, Muhammad Hayat, MD1, Marjan Haider, MD2, Manesh Kumar Gangwani, MD3, Muhammad Aziz, MD4, Umar Hayat, MD5, Umer Farooq, MD6, Nasir Saleem, MD7, Faisal Kamal, MD8. P0019 - Laser-Cut-Type vs Braided-Type Self-Expandable Metallic Stents for Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Vanderbilt University Medical Center, Nashville, TN; 2Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 3University of Toledo, Toledo, OH; 4Bon Secours Mercy, Toledo, OH; 5Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 6SSM Health Saint Louis University Hospital, St. Louis, MO; 7Indiana University School of Medicine, Indianapolis, IN; 8Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Self-expandable metallic stents (SEMS) are widely used for malignant biliary obstruction (MBO). Laser cut and braided stents are two commonly used types of SEMS, and it is unclear if one stent type is superior to the other. We conducted a systematic review and meta-analysis to compare outcomes of these two stent types in patients with MBO.
Methods: Several databases were reviewed from inception to May 24th, 2024 to identify studies comparing outcomes of laser-cut and braided-type SEMS in patients with MBO. The databases searched included PubMed, Web of Science Core Collection, Embase, and the Cochrane Database of Systematic Reviews. Our outcomes of interest included technical success, clinical success, mean procedure time and adverse events such as pancreatitis, cholecystitis, stent migration and recurrent biliary obstruction. We calculated risk ratios (RRs) with 95% confidence intervals (CIs) for all dichotomous variables and mean difference with 95% CI for continuous variables. Data was analyzed using random effect model. Heterogeneity was assessed using I2 statistic.
Results: Four studies comprising 430 patients (Laser-cut 210 and braided type 220) met the inclusion criteria. We found no significant difference in rate of technical success, RR (95% CI): 1.00 (0.98,1.02), p=0.96, and clinical success, RR (95% CI): 1.01 (0.97, 1.04), p=0.68 between groups (Figure 1A and B). There was no significant difference in rate of adverse events between groups, RR (95% CI): 1.06 (0.60,1.90), p=0.84 (Figure 3). There was no significant difference in rate of adverse events between groups, such as pancreatitis, RR (95% CI): 01.26(0.59, 2.71), p=0.55; cholecystitis, RR (95% CI): 0.76 (0.30, 1.95), p=0.57; stent migration, RR (95% CI): 1.43(0.32,6.38), p=0.64 and recurrent biliary obstruction RR (95% CI): 1.18 (0.64, 2.16), p=0.60 (Figure 4,5). We found no significant difference in procedure time between groups, MD (95% CI): 0.84(-4.29,5.99), p=0.75 (Figure 6,7).
Discussion: We found no significant difference in outcomes between laser cut and braided stents in patients with MBO. Large multicenter, randomized controlled trials comparing the two stent types are required to further validate these findings.
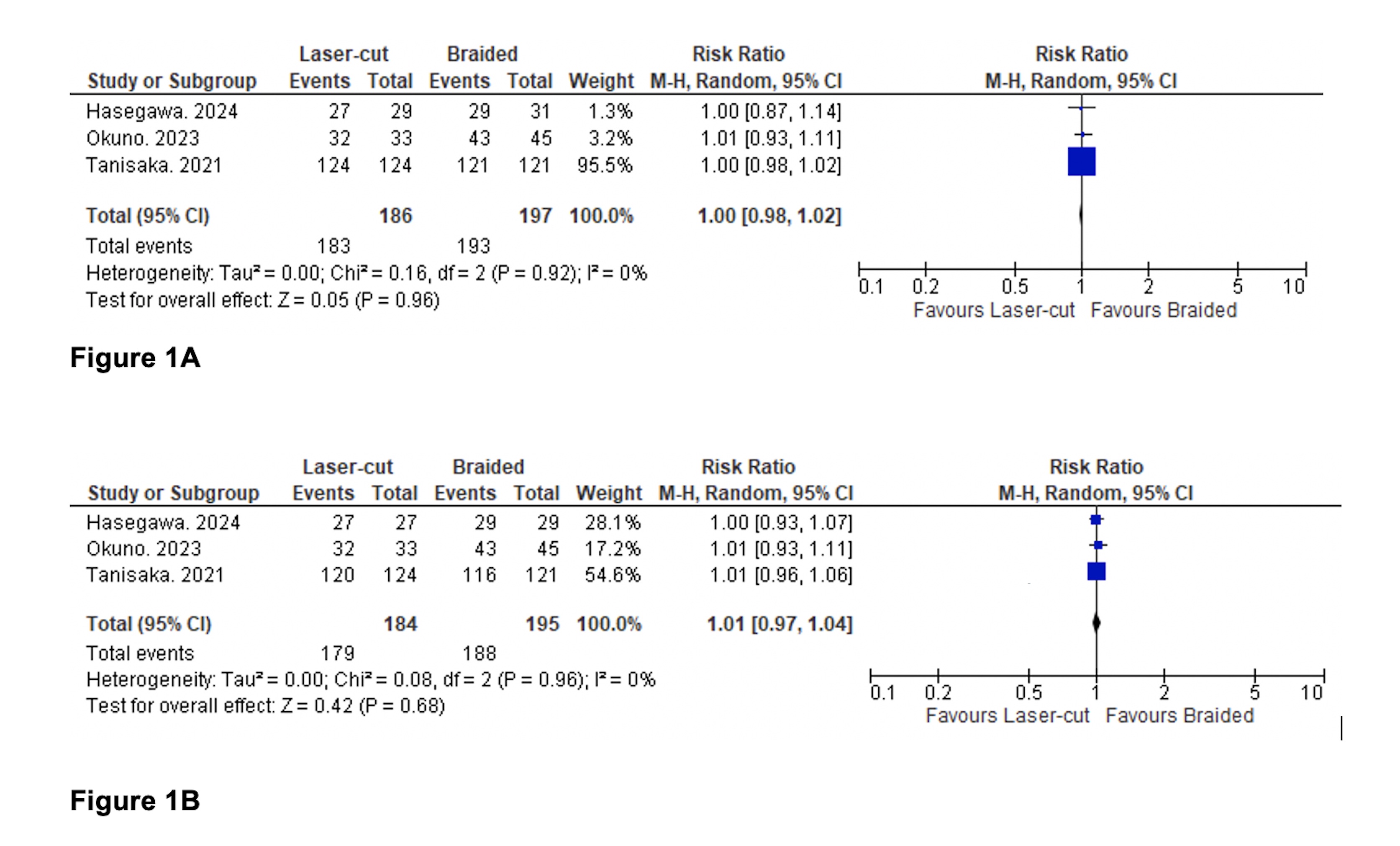
Figure: Comparison of technical success (Figure 1A) and clinical success (Figure 1B) between groups.
Disclosures:
Aamir Saeed indicated no relevant financial relationships.
Saira Yousuf indicated no relevant financial relationships.
Muhammad Hayat indicated no relevant financial relationships.
Marjan Haider indicated no relevant financial relationships.
Manesh Kumar Gangwani indicated no relevant financial relationships.
Muhammad Aziz indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Nasir Saleem indicated no relevant financial relationships.
Faisal Kamal indicated no relevant financial relationships.
Aamir Saeed, MD1, Saira Yousuf, MD1, Muhammad Hayat, MD1, Marjan Haider, MD2, Manesh Kumar Gangwani, MD3, Muhammad Aziz, MD4, Umar Hayat, MD5, Umer Farooq, MD6, Nasir Saleem, MD7, Faisal Kamal, MD8. P0019 - Laser-Cut-Type vs Braided-Type Self-Expandable Metallic Stents for Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
