Sunday Poster Session
Category: Biliary/Pancreas
P0022 - The Impact of ERCP on Clinical Outcomes During the Management of Encapsulated Pancreatic Collections - A Retrospective Observational Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Shruti Kulkarni, MD
University of South Florida
Tampa, FL
Presenting Author(s)
Shruti Kulkarni, MD, Melanie Cabezas, MD, Pushpak Taunk, MD, Jonathan Hilal, MD
University of South Florida, Tampa, FL
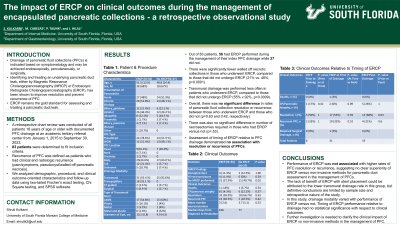
Introduction: Drainage of pancreatic fluid collections (PFC) is indicated based on size and symptomatology and may be achieved endoscopically, percutaneously, or surgically. Identifying and treating an underlying pancreatic duct leak, either by Magnetic Resonance Cholangiopancreatography (MRCP) or Endoscopic Retrograde Cholangiopancreatography (ERCP), has been shown to improve resolution and prevent recurrence of PFC. ERCP remains the gold standard for assessing and treating a pancreatic duct leak. Herein, we investigate the influence of utilization of ERCP on clinical outcomes following PFC treatment.
Methods: A retrospective chart review was conducted of all patients 18 years of age or older with documented PFC drainage at an academic tertiary referral center from January 1, 2015 to September 30, 2023. Eighty-three patients were determined to fit inclusion criteria. Recurrence of PFC was defined as patients who had clinical and radiologic recurrence (pain/symptoms, pseudocyst/walled off pancreatic necrosis). We analyzed demographic, procedural, and clinical outcome-oriented characteristics and follow-up data using two-tailed Fischer’s exact testing, Chi Square testing, and SPSS software.
Results: Eighty-three patients were analyzed. Fifty-six patients were determined to have had ERCP performed during the management of their index PFC drainage, while 27 did not. Fewer patients with walled off necrosis underwent ERCP during management of their PFC (p=0.0001). A higher proportion of patients who had transmural drainage did not undergo ERCP (p=0.0009). Overall, there was no significant difference in rates of pancreatic fluid collection resolution or recurrence between those who underwent ERCP and those who did not (p=0.63, 0.42). There was also no significant difference in number of necrosectomies required in those who had ERCP versus not (p=.53). Assessment of timing of ERCP relative to PFC drainage demonstrated no association with resolution or recurrence of PFCs.
Discussion: Performance of ERCP was not associated with higher rates of PFC resolution or recurrence, suggesting no clear superiority of ERCP versus non-invasive methods for pancreatic duct assessment in the management of PFCs. In this study, drainage modality varied with performance of ERCP versus not. Timing of ERCP performance relative to drainage had no statistical significance with respect to clinical outcomes. Further investigation is needed to clarify the clinical impact of ERCP vs non-invasive methods in the management of PFC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shruti Kulkarni, MD, Melanie Cabezas, MD, Pushpak Taunk, MD, Jonathan Hilal, MD. P0022 - The Impact of ERCP on Clinical Outcomes During the Management of Encapsulated Pancreatic Collections - A Retrospective Observational Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of South Florida, Tampa, FL
Introduction: Drainage of pancreatic fluid collections (PFC) is indicated based on size and symptomatology and may be achieved endoscopically, percutaneously, or surgically. Identifying and treating an underlying pancreatic duct leak, either by Magnetic Resonance Cholangiopancreatography (MRCP) or Endoscopic Retrograde Cholangiopancreatography (ERCP), has been shown to improve resolution and prevent recurrence of PFC. ERCP remains the gold standard for assessing and treating a pancreatic duct leak. Herein, we investigate the influence of utilization of ERCP on clinical outcomes following PFC treatment.
Methods: A retrospective chart review was conducted of all patients 18 years of age or older with documented PFC drainage at an academic tertiary referral center from January 1, 2015 to September 30, 2023. Eighty-three patients were determined to fit inclusion criteria. Recurrence of PFC was defined as patients who had clinical and radiologic recurrence (pain/symptoms, pseudocyst/walled off pancreatic necrosis). We analyzed demographic, procedural, and clinical outcome-oriented characteristics and follow-up data using two-tailed Fischer’s exact testing, Chi Square testing, and SPSS software.
Results: Eighty-three patients were analyzed. Fifty-six patients were determined to have had ERCP performed during the management of their index PFC drainage, while 27 did not. Fewer patients with walled off necrosis underwent ERCP during management of their PFC (p=0.0001). A higher proportion of patients who had transmural drainage did not undergo ERCP (p=0.0009). Overall, there was no significant difference in rates of pancreatic fluid collection resolution or recurrence between those who underwent ERCP and those who did not (p=0.63, 0.42). There was also no significant difference in number of necrosectomies required in those who had ERCP versus not (p=.53). Assessment of timing of ERCP relative to PFC drainage demonstrated no association with resolution or recurrence of PFCs.
Discussion: Performance of ERCP was not associated with higher rates of PFC resolution or recurrence, suggesting no clear superiority of ERCP versus non-invasive methods for pancreatic duct assessment in the management of PFCs. In this study, drainage modality varied with performance of ERCP versus not. Timing of ERCP performance relative to drainage had no statistical significance with respect to clinical outcomes. Further investigation is needed to clarify the clinical impact of ERCP vs non-invasive methods in the management of PFC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shruti Kulkarni indicated no relevant financial relationships.
Melanie Cabezas indicated no relevant financial relationships.
Pushpak Taunk: Boston Scientific – Consultant. Neptune Medical – Consultant.
Jonathan Hilal indicated no relevant financial relationships.
Shruti Kulkarni, MD, Melanie Cabezas, MD, Pushpak Taunk, MD, Jonathan Hilal, MD. P0022 - The Impact of ERCP on Clinical Outcomes During the Management of Encapsulated Pancreatic Collections - A Retrospective Observational Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
