Sunday Poster Session
Category: Biliary/Pancreas
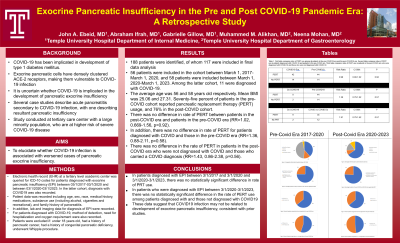
P0023 - Exocrine Pancreatic Insufficiency in the Pre and Post COVID-19 Pandemic Era: A Retrospective Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

John Ebeid, MD
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
John Ebeid, MD1, Abraham Ifrah, MD1, Gabrielle Gillow, MD1, Muhammed Alikhan, MD2, Neena Mohan, MD1
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: COVID19 causes severe pancreatic inflammation through invasion and destruction of pancreatic islet cells via the ACE-2 receptor. Pancreatic exocrine cells also contain this receptor and infection can theoretically result in exocrine pancreatic insufficiency. There is a dearth of studies assessing the relation between COVID19 infection and the subsequent development of pancreatic insufficiency. This study aims to elucidate any such association in an urban tertiary medical center.
Methods: Electronic health record (EHR) at a tertiary level academic center was queried for ICD-10 codes for patients diagnosed with pancreatic insufficiency (PI) between 03/1/2017-03/1/2020 and 03/1/2020-03/1/2023. Patient demographic data was recorded: age, sex, race, medical history, medications, recreational substance use, and family history of pancreatitis. For patients diagnosed with COVID19, method of detection, hospitalization and oxygen use were recorded. Patients were excluded if: under 18 years old, had pancreatic cancer, had congenital pancreatic deficiency, or underwent Whipple procedure.
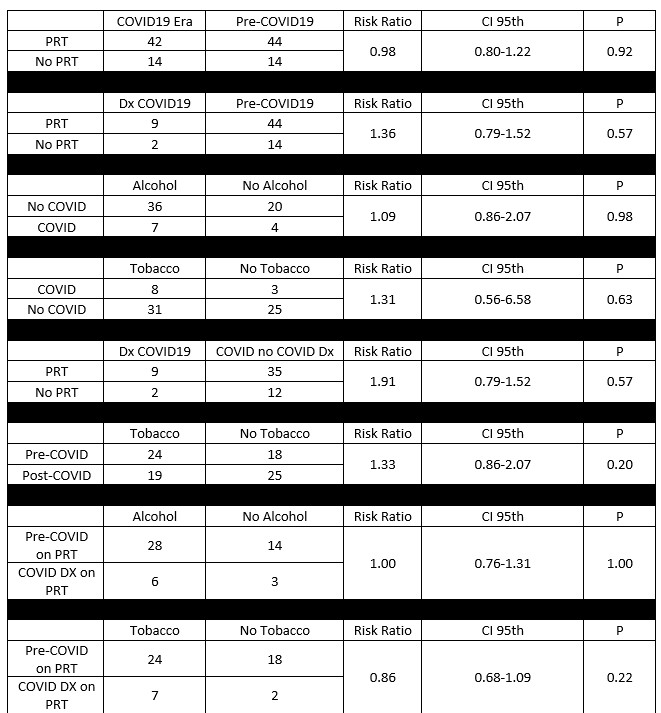
Results: 117 patients were included. 56 patients were included in the cohort between 03/01/2017-03/01/2020, and 58 patients were included between 03/01/2020-03/01/2023. The average age was 56 and 58 years old respectively with mean BMI 25.06 and 27.31. 11 patients were diagnosed with COVID-19. Seventy-five percent of patients in the pre-COVID cohort reported pancreatic replacement therapy (PRT) use, and 76% in the post-COVID cohort. There was no difference in rate of PRT between patients in the post-COVID era and patients in the pre-COVID era (RR=0.98, 0.80-1.22, p=0.92), in rate of PRT for patients diagnosed with COVID and those in the pre-COVID era (RR=1.36, 0.79-1.48, p=0.63), or in the rate of PRT in patients in the post-COVID era who were not diagnosed with COVID and those diagnosed with COVID (RR=1.43, 0.86-2.38, p=0.56). Average BMI was significantly different between patients diagnosed with COVID and those in the pre-COVID era who received PRT (24.4±1.57 vs. 32.3±5.8, p< 0 .0001).
Discussion: In patients diagnosed with PI between 3/1/2017 and 3/1/2020 and 3/1/2020-3/1/2023, there was no significant difference in rate of PRT use. In patients diagnosed with PI between 3/1/2020-3/1/2023, there was no difference in the rate of PRT use between patients diagnosed with COVID19 and those who were not. These data suggest that COVID19 infection may not be related to development of exocrine pancreatic insufficiency.
Disclosures:
John Ebeid, MD1, Abraham Ifrah, MD1, Gabrielle Gillow, MD1, Muhammed Alikhan, MD2, Neena Mohan, MD1. P0023 - Exocrine Pancreatic Insufficiency in the Pre and Post COVID-19 Pandemic Era: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: COVID19 causes severe pancreatic inflammation through invasion and destruction of pancreatic islet cells via the ACE-2 receptor. Pancreatic exocrine cells also contain this receptor and infection can theoretically result in exocrine pancreatic insufficiency. There is a dearth of studies assessing the relation between COVID19 infection and the subsequent development of pancreatic insufficiency. This study aims to elucidate any such association in an urban tertiary medical center.
Methods: Electronic health record (EHR) at a tertiary level academic center was queried for ICD-10 codes for patients diagnosed with pancreatic insufficiency (PI) between 03/1/2017-03/1/2020 and 03/1/2020-03/1/2023. Patient demographic data was recorded: age, sex, race, medical history, medications, recreational substance use, and family history of pancreatitis. For patients diagnosed with COVID19, method of detection, hospitalization and oxygen use were recorded. Patients were excluded if: under 18 years old, had pancreatic cancer, had congenital pancreatic deficiency, or underwent Whipple procedure.
Results: 117 patients were included. 56 patients were included in the cohort between 03/01/2017-03/01/2020, and 58 patients were included between 03/01/2020-03/01/2023. The average age was 56 and 58 years old respectively with mean BMI 25.06 and 27.31. 11 patients were diagnosed with COVID-19. Seventy-five percent of patients in the pre-COVID cohort reported pancreatic replacement therapy (PRT) use, and 76% in the post-COVID cohort. There was no difference in rate of PRT between patients in the post-COVID era and patients in the pre-COVID era (RR=0.98, 0.80-1.22, p=0.92), in rate of PRT for patients diagnosed with COVID and those in the pre-COVID era (RR=1.36, 0.79-1.48, p=0.63), or in the rate of PRT in patients in the post-COVID era who were not diagnosed with COVID and those diagnosed with COVID (RR=1.43, 0.86-2.38, p=0.56). Average BMI was significantly different between patients diagnosed with COVID and those in the pre-COVID era who received PRT (24.4±1.57 vs. 32.3±5.8, p< 0 .0001).
Discussion: In patients diagnosed with PI between 3/1/2017 and 3/1/2020 and 3/1/2020-3/1/2023, there was no significant difference in rate of PRT use. In patients diagnosed with PI between 3/1/2020-3/1/2023, there was no difference in the rate of PRT use between patients diagnosed with COVID19 and those who were not. These data suggest that COVID19 infection may not be related to development of exocrine pancreatic insufficiency.
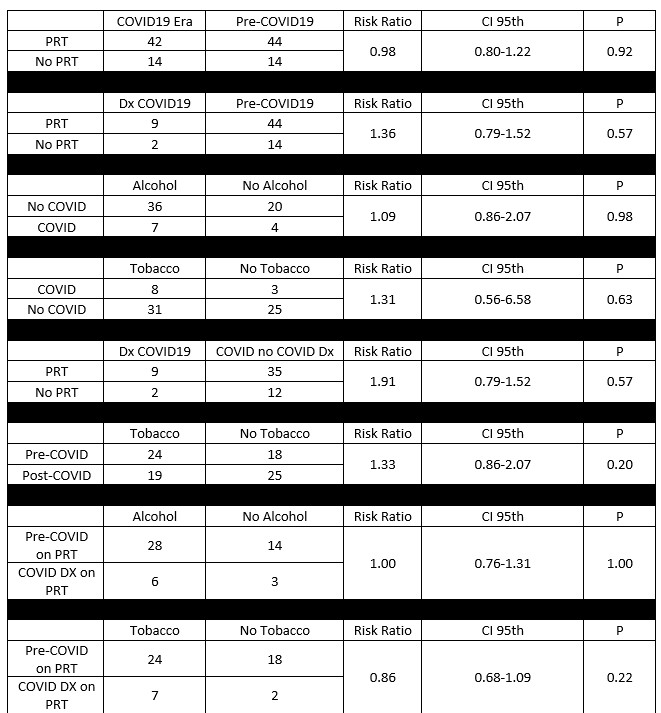
Figure: Table 1. Risk ratios of several variables and comparisons between cohorts including patients in the pre-COVID19 era and those in the post-COVID19 era. Use of alcohol, tobacco and pancreatic replacement therapy are compared. Dx = diagnosed, PRT = Pancreatic replacement therapy, CI 95th = Confidence Interval 95th percentile, No COVID = post-covid era with no diagnosis of COVID19.
Disclosures:
John Ebeid indicated no relevant financial relationships.
Abraham Ifrah indicated no relevant financial relationships.
Gabrielle Gillow indicated no relevant financial relationships.
Muhammed Alikhan indicated no relevant financial relationships.
Neena Mohan indicated no relevant financial relationships.
John Ebeid, MD1, Abraham Ifrah, MD1, Gabrielle Gillow, MD1, Muhammed Alikhan, MD2, Neena Mohan, MD1. P0023 - Exocrine Pancreatic Insufficiency in the Pre and Post COVID-19 Pandemic Era: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
