Sunday Poster Session
Category: Biliary/Pancreas
P0025 - The Intersection of Healthcare Disparities and Cholangitis Management: A National Database Evaluation of 30-Day Readmission Rates
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
- RR
Rajmohan Rammohan, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA
Nassau University Medical Center, East Meadow, NY
Introduction: Predicting 30-day readmission for cholangitis patients hinges on comprehending the impact of comorbidities and length of hospital stay. This predictive endeavor entails analyzing how underlying conditions such as diabetes, cirrhosis, or malignancies influence readmission risk alongside evaluating the duration of hospitalization. By discerning these factors' interplay, healthcare practitioners can tailor interventions, optimize post-discharge care plans, and ultimately mitigate readmission rates, fostering improved patient outcomes and resource allocation efficiency within healthcare systems.
Methods: From 2019 to 2022, we analyzed the Nationwide Readmission Database, focusing on 1,048,576 adults readmitted within 30 days with a primary diagnosis of Cholangitis. We used logistic regression to explore factors affecting 30-day readmission rates in a subset of 4,259 patients, considering demographics and clinical comorbidities. We checked for multicollinearity and adjusted the dataset before fitting the logistic model using stats models. The analysis highlighted significant predictors of readmission, providing valuable insights for reducing future readmission risks.
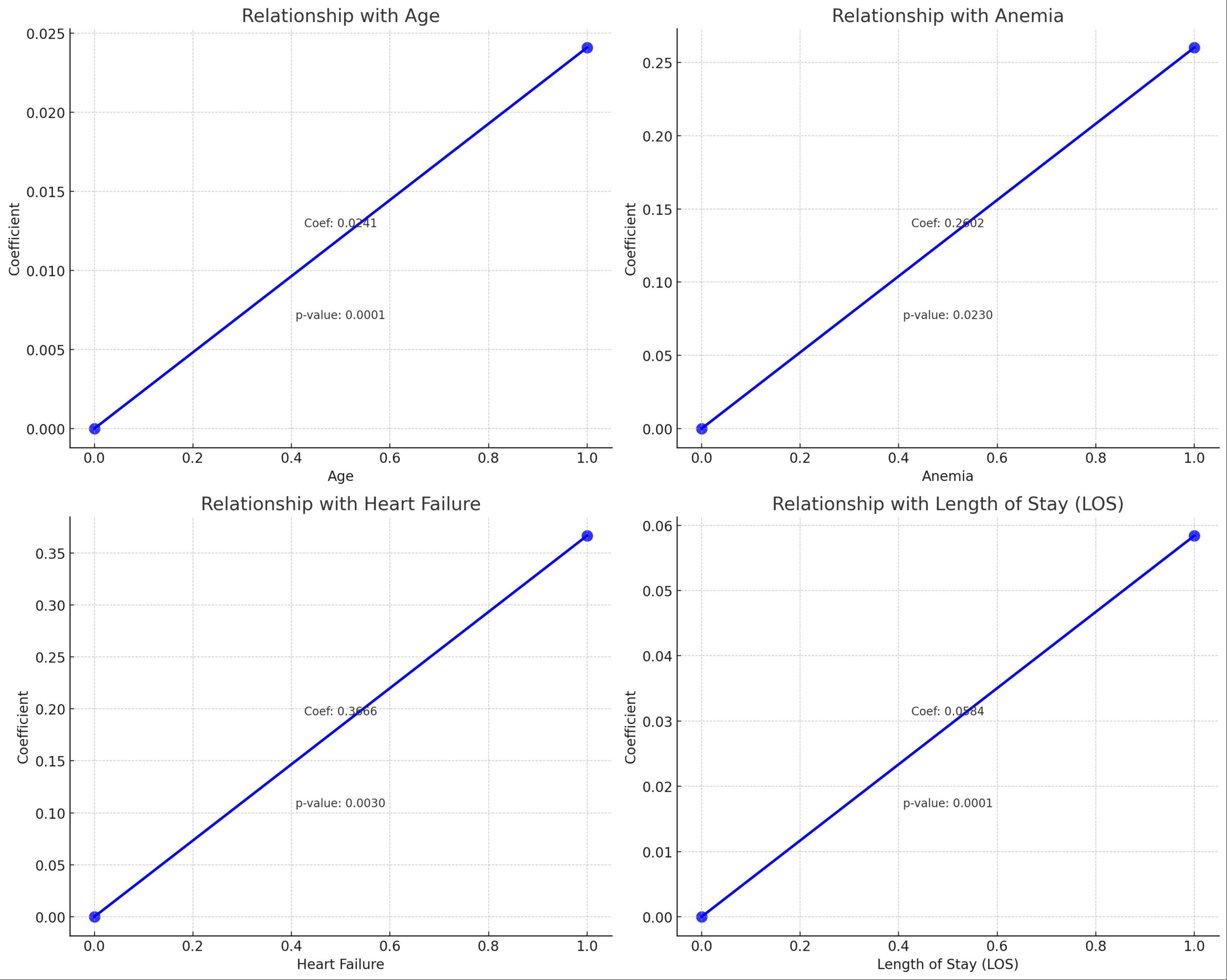
Results: This study examined 4,259 cholangitis patients to identify factors impacting 30-day readmission rates using logistic regression. Key predictors included age (coefficient 0.0241, p < 0.0001), hyperlipidemia (HLD) showing a protective effect (coefficient -0.2431, p = 0.011), anemia (coefficient 0.2602, p = 0.023), heart failure (coefficient 0.3666, p = 0.003), and length of stay (LOS) (coefficient 0.0584, p < 0.0001). Each additional year of age, day of hospital stay, and conditions like anemia and heart failure increased readmission odds, underscoring the need for targeted interventions and personalized care strategies to mitigate readmission risks
Discussion: Our study highlights how comorbidities and length of stay (LOS) predict 30-day readmissions in cholangitis patients. Logistic regression shows that older age, extended LOS, and conditions like anemia and heart failure increase readmission risks. Targeted discharge planning and tailored follow-up for high-risk patients may reduce these rates. The role of hyperlipidemia (HLD) as a protective factor needs further study. Focusing on these predictors can enhance patient outcomes and reduce readmissions
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P0025 - The Intersection of Healthcare Disparities and Cholangitis Management: A National Database Evaluation of 30-Day Readmission Rates, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Predicting 30-day readmission for cholangitis patients hinges on comprehending the impact of comorbidities and length of hospital stay. This predictive endeavor entails analyzing how underlying conditions such as diabetes, cirrhosis, or malignancies influence readmission risk alongside evaluating the duration of hospitalization. By discerning these factors' interplay, healthcare practitioners can tailor interventions, optimize post-discharge care plans, and ultimately mitigate readmission rates, fostering improved patient outcomes and resource allocation efficiency within healthcare systems.
Methods: From 2019 to 2022, we analyzed the Nationwide Readmission Database, focusing on 1,048,576 adults readmitted within 30 days with a primary diagnosis of Cholangitis. We used logistic regression to explore factors affecting 30-day readmission rates in a subset of 4,259 patients, considering demographics and clinical comorbidities. We checked for multicollinearity and adjusted the dataset before fitting the logistic model using stats models. The analysis highlighted significant predictors of readmission, providing valuable insights for reducing future readmission risks.
Results: This study examined 4,259 cholangitis patients to identify factors impacting 30-day readmission rates using logistic regression. Key predictors included age (coefficient 0.0241, p < 0.0001), hyperlipidemia (HLD) showing a protective effect (coefficient -0.2431, p = 0.011), anemia (coefficient 0.2602, p = 0.023), heart failure (coefficient 0.3666, p = 0.003), and length of stay (LOS) (coefficient 0.0584, p < 0.0001). Each additional year of age, day of hospital stay, and conditions like anemia and heart failure increased readmission odds, underscoring the need for targeted interventions and personalized care strategies to mitigate readmission risks
Discussion: Our study highlights how comorbidities and length of stay (LOS) predict 30-day readmissions in cholangitis patients. Logistic regression shows that older age, extended LOS, and conditions like anemia and heart failure increase readmission risks. Targeted discharge planning and tailored follow-up for high-risk patients may reduce these rates. The role of hyperlipidemia (HLD) as a protective factor needs further study. Focusing on these predictors can enhance patient outcomes and reduce readmissions
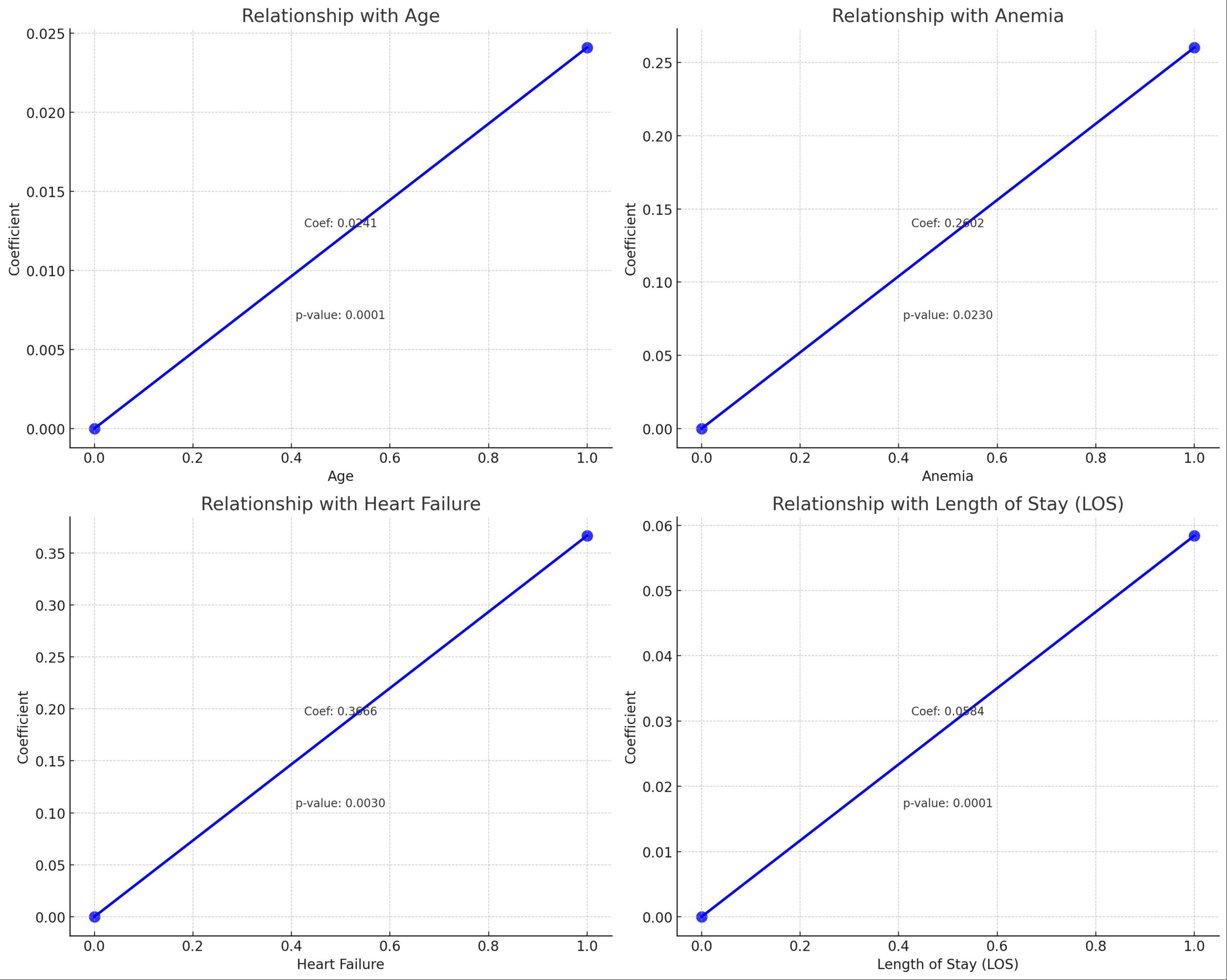
Figure: Scattered plot analysis of 30 day readmission in patient with cholangitis
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Mohan Ram Mohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Sai Greeshma Magam indicated no relevant financial relationships.
Melvin Joy indicated no relevant financial relationships.
Dilman Natt indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Winghang Lau indicated no relevant financial relationships.
Abhishek Tadikonda indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Krishnaiyer Subramani indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P0025 - The Intersection of Healthcare Disparities and Cholangitis Management: A National Database Evaluation of 30-Day Readmission Rates, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
